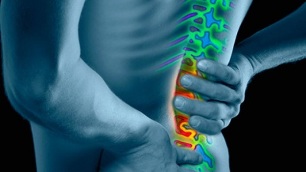
Contrary to popular belief, osteochondrosis of the spine is not considered part of the aging process. Elastic discs between the vertebrae are responsible for bending and lengthening the back, like shock absorbers. Over time, they wear out and no longer provide the full range of motion. With age, daily stress on the spine and accidental injuries, including minor ones, can damage the discs on the back and lead to osteochondrosis of the lumbar spine.
Who is affected by this lower back disease?

In most cases, the first symptoms of osteochondrosis of the lumbar spine appear at the age of 11-12. The disease manifests itself vividly until the age of sixteen, but the most severe course and frequent complications occur between the ages of 15 and 20.
Children under the age of 15 rarely have severe forms of osteochondrosis, which is somehow related to the excellent condition of their musculoskeletal system in general, and the spine in particular. In addition, the disease takes time to develop, and on average it takes five years.
Fortunately, these diseases are much easier to treat in children than in adults.
Symptoms
Reflex syndromes
- Cervicalgia- variously manifested neck pain (pulling, tingling, cracking), a feeling of "creeping" in the neck muscles, as well as reduced mobility and flexibility of the neck.
- Lumbagois a sharp, sharp pain in the lumbar region, which may be accompanied by numbness or swelling. Instead of the word "lumbago", the words "lumbodynia" or "lumboischialgia" may be used.
- Thoracalgia- pains of various natures in the chest, shoulders and ribs, which are constantly present or occur during body movements.
Compression syndromes
Occurrence of pain syndrome in osteochondrosis of the lumbar spine is a consequence of:
- Compression of root structures (radiculopathy).
- Spinal cord compression (myelopathy).
- Spinal cord injury due to impaired blood supply.
- Narrowing (stenosis) of arteries and veins (compressive-vascular myelochemia).
Disease detection methods
Differential Diagnostics
Not every disorder can be diagnosed with a simple laboratory test. Many conditions cause similar symptoms. For example, many infections cause fever, headache, and fatigue.
Many mental disorders are caused by:

- sadness;
- concern;
- sleep problems.
The differential diagnosis identifies possible disorders that cause symptoms. Typically, this diagnosis is based on several tests. These tests may rule out conditions and / or determine if you need additional tests.
Differential diagnosis is used to diagnose physical or mental health problems that cause similar symptoms.
Differential diagnosis is also often used in the field of psychiatry / psychology, where a patient who has symptoms of several diseases can be given two different diagnoses. For example, a patient diagnosed with bipolar disorder may also be differentially diagnosed with borderline personality disorder given the similarity of symptoms in both conditions.
Who is diagnosed more often?
If earlier the disease was diagnosed in sick people after the age of 45, today about 27% of adolescents suffer from osteochondrosis of one degree or another.
Such a large spread of the disease is understandable - children began to spend a lot of time in a sitting position, including because of computers and the Internet. Is it bad? Time will tell, but the fact remains - the pay for an inactive lifestyle is high, and osteochondrosis is far from the worst disease that can occur with such a lifestyle, but it is the most common (after obesity).
How to define the disease and its degree?
First
In the normal state, the intervertebral discs are constantly renewed, but it happens that the process slows down and a disease like 1st degree osteochondrosis occurs.
There are many reasons for this:
- obese;
- metabolic disorders;
- immunity and so on.
Unfortunately, the instability of pain of a certain degree of disease is influenced by the fact that many people neglect diagnosis and treatment and try to cure the pain themselves. To do this, use ointments and various tinctures. But this is the biggest mistake.
First degree osteochondrosis of the lumbar spine can be easily cured by contacting a good specialist and performing a series of simple actions.
Grade 1 osteochondrosis is the seal of intervertebral cartilage in the lumbar region. The main symptom at this stage is less pain when turning or bending. Sometimes the symptoms are more acute and short-lived due to sudden movements or significant efforts.
Other
A pronounced symptom of the disease is pain in the lumbar region that intensifies with each movement. The pain may radiate more along the spine.
In osteochondrosis, the pain can radiate to the lower extremities.
The second stage of osteochondrosis is characterized by such severe pain that it manifests itself even when coughing.
Additional symptoms are associated with pinched nerve endings:
- The sensitivity of the lower limbs changes. The main signs are: pain, numbness of the legs, high or too low level of sensitivity of the skin of the lower extremities.
- Limited mobility. A person suffering from osteochondrosis (grade 2) notices that as the disease progresses, it becomes very difficult to move.
- Increased fatigue and constant drowsiness. The patient has chronic fatigue, accompanied by irritability. This symptom is explained by a pain syndrome that constantly torments a person.
- Problematic urination and pain in the kidney area.
Third

By the time the patient reached stage 3, his posture had changed significantly. In more advanced cases, bone deformation occurs. In this phase of osteochondrosis of the lumbar spine, there is an obvious worsening of the general physical and / or mental condition of the patient and a deep loss of energy.
The third phase is characterized by the appearance of narrowing of the intervertebral foramen compared to the previous changes. Hernias of the intervertebral discs were created, and the vessels of the neck and muscles were damaged. The patient has dizziness, pain in the back of the head.
Fourth
The terminal phase occurs when the intervertebral disc degenerates and the disk space is destroyed. At this stage, the thinning of the disc reaches its maximum or, worse, disappears completely. Postural imbalance is acute, and movement and flexibility are extremely limited.
Stage 4 osteochondrosis of the lumbar spine is often characterized by severe pain and a greater degree of deterioration of physical and / or mental condition. There is also a permanent loss of growth and energy levels. Phase 4 is usually considered irreversible.
Doctor's consultation
Which doctor should I contact?
When independent methods of treatment cease to produce an analgesic effect, the patient begins to ask himself the question: which doctor treats osteochondrosis? The first person you can contact to treat lumbar spine osteochondria is your local therapist. But in this situation, he plays the role of a dispatcher, because he will not be able to prescribe a complete treatment - that is not his specialization.
They will most likely send you to a neurologist. This specialist will conduct the necessary research and help build a treatment program. The therapist can also refer you to a vertebrologist. This doctor deals directly with spinal diseases.
Scales and tests
Quality of Life Assessment

Such a generalized characteristic as quality of life is especially important for a group of patients with comorbid diseases, because they can affect the effectiveness of treatment. This is especially important for comparing the results of several studies, economic analysis, and for understanding the problem as a whole.
Methods for assessing quality of life include:
- Questionnaire on quality of life for the most modern.
- Roland-Morris questionnaire.
- Stratford scale.
- Quebec Back Pain Scale - a questionnaire on how back pain affects your daily life).
Pain scales
Pain is an unpleasant sensation and emotional experience associated with tissue damage. Its purpose is to allow the body to react and prevent further tissue damage.
Methods for assessing pain syndrome include:
- He won the Corfu scale for assessing chronic pain.
- McGill Pain Questionnaire.
- Verbal pain scale.
Assessment of treatment outcomes
- McNab's scale of subjective evaluation.
- Patient satisfaction scale.
- Prolo scale of functional and economic outcomes.
- Lumbosacral outcome scale.
- Nurik's scales.
Hardware Test
X-ray
X-rays provide detailed bone structures of the spine and are used to rule out back pain that results from:
- Spondylolisthesis.
- Tumors.
- Cracks.
Calcium in the bone blocks the penetration of X-rays, and the image of the bones is perceived as a shadow on the film. X-rays provide excellent visibility of all the details because the bone is mostly made of calcium. However, the discs and nerve roots do not contain calcium, so X-rays do not capture images of these structures. X-rays, therefore, cannot be used to diagnose lumbar disc herniation or other causes of nerve constriction.
X-rays should not be taken on pregnant women.
Complications and possible consequences
Complications and possible consequences of lumbar osteochondrosis include:
- Radiculopathy is a condition characterized by nerve root disease.
- Muscle weakness - Common symptoms include fever, fatigue, flu-like symptoms, paraesthesia, weight loss and changes in consciousness.
- Neurogenic bladder - problems with the nerves that control the bladder and urination
- Damage to lower motor neurons.
- Raynaud's phenomenon is a condition in which cramps occur, narrowing the capillaries of the fingers and toes.
- Pain in neck, back, legs.
Treatment
Treatment can vary depending on the severity of your symptoms and how much they limit your daily activities.
Here are some treatments your doctor may prescribe based on your pain:
- Non-surgical treatment- not all patients with osteochondrosis need surgery. For mild to moderate pain, more conservative treatments.
- Spondylodesis- surgical intervention in the treatment of osteochondrosis.
Prevention

Prevention of osteochondrosis of the lumbar segment is the removal of risk factors that lead to this disease. Removal of factors is the main preventive measure.
Physical activity is normalized, the back muscles are strengthened, the maximum load on the lower back is prevented, the development of diseases that lead to lower back pain is prevented, all this is prophylaxis for the prevention of lumbar osteochondrosis symptoms.
Moderate exercise, lifestyle changes, and a good diet can help prevent painful and disabling symptoms.
If you notice symptoms of lumbar spine osteochondrosis, do not pinch them and consult a doctor immediately. The disease detected in time is easier to treat and passes without consequences.























